Background
Hemorrhoids are one of the most common causes of anal pathology. Subsequently, hemorrhoids are blamed for virtually any anorectal complaint by patients and medical professionals alike. Confusion often arises because the term "hemorrhoid" has been used to refer to both normal anatomical structures and pathological structures. In the context of this article, "hemorrhoids" refers to the pathological presentation of hemorrhoidal venous cushions.
Hemorrhoidal venous cushions are normal structures of the anorectum and are universally present unless a prior intervention has taken place. Because of their rich vascular supply, highly sensitive location, and tendency to engorge and prolapse, they are common causes of anal pathology.1 Symptoms can range from mildly bothersome, such as pruritus, to quite concerning, such as rectal bleeding, and while it is a common condition diagnosed in clinical practice, many patients are too embarrassed to ever seek treatment. Consequently, the true prevalence of pathologic hemorrhoids is not known.2
Even though hemorrhoids are responsible for a large portion of anorectal complaints, it is important to rule out more serious conditions, such as other causes of GI bleeding, before reflexively attributing symptoms to hemorrhoids.3
Pathophysiology
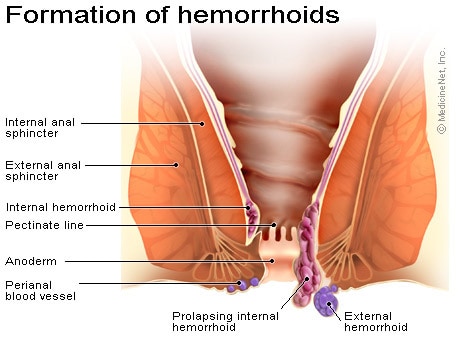
Hemorrhoidal venous cushions are a normal part of the human anorectum and arise from subepithelial connective tissue within the anal canal.
Present in utero, these cushions surround and support distal anastomoses between the superior rectal arteries and the superior, middle, and inferior rectal veins. They also contain a subepithelial smooth muscle layer, contributing to the bulk of the cushions. Normal hemorrhoidal tissue accounts for approximately 15-20% of resting anal pressure and provides important sensory information, enabling the differentiation between solid, liquid, and gas.
Most people contain 3 of these cushions. Although classically described as lying in the right posterior (most common), right anterior, and left lateral positions, this combination is found in only 19% of patients. Hemorrhoids can be found at any position within the rectum.
Hemorrhoids are classified by their anatomic origin within the anal canal and by their position relative to the dentate line.
- Internal hemorrhoids develop above the dentate line from embryonic endoderm. They are covered by the simple columnar epithelium of anal mucosa and lack somatic sensory innervation and are therefore painless.
- External hemorrhoids develop from ectoderm and arise distal to the dentate line. They are covered by stratified squamous epithelium and receive somatic sensory innervation from the inferior rectal nerve rendering them painful when irritated.
- Mixed hemorrhoids are confluent internal and external hemorrhoids.
Venous drainage of hemorrhoidal tissue mirrors embryologic origin:
- Internal hemorrhoids drain through the superior rectal vein into the portal system.
- External hemorrhoids drain through the inferior rectal vein into the inferior vena cava.
- Rich anastomoses exist between these 2 and the middle rectal vein, connecting the portal and systemic circulations.
Most symptoms arise from enlarged internal hemorrhoids. Abnormal swelling of the anal cushions causes dilatation and engorgement of the arteriovenous plexuses. This leads to stretching of the suspensory muscles and eventual prolapse of rectal tissue through the anal canal. The engorged anal mucosa is easily traumatized, leading to rectal bleeding that is typically bright red due to high blood oxygen content within the arteriovenous anastomoses. Prolapse leads to soiling and mucus discharge (triggering pruritus) and predisposes to incarceration and strangulation.
Most clinicians use the grading system proposed by Banov et al in 1985, which classifies internal hemorrhoids by their degree of prolapse into the anal canal. This system both correlates with symptoms and guides therapeutic approaches.
- Grade I hemorrhoids project into the anal canal and often bleed but do not prolapse.
- Grade II hemorrhoids may protrude beyond the anal verge with straining or defecating but reduce spontaneously when straining ceases.
- Grade III hemorrhoids protrude spontaneously or with straining and require manual reduction.
- Grade IV hemorrhoids chronically prolapse and cannot be reduced. They usually contain both internal and external components and may present with acute thrombosis or strangulation.
Frequency
United States
Prevalence of symptomatic hemorrhoids is estimated at 4.4% in the general population.
Race
Patients presenting with hemorrhoidal disease are more frequently Caucasian, from higher socioeconomic status, and from rural areas.
Sex
No predilection is known, although men are more likely to seek treatment. However, pregnancy causes physiologic changes that predispose women to developing symptomatic hemorrhoids. As the gravid uterus expands, it compresses the inferior vena cava, causing decreased venous return and distal engorgement.
Age
External hemorrhoids occur more commonly in young and middle-aged adults than in older adults. The prevalence of hemorrhoids increases with age, with a peak in persons aged 45-65 years.
The treatment of hemorrhoids is one area in which alternative therapy is gaining acceptance with conventional physicians. Several therapies offer natural pain relief from hemorrhoids and aid in preventing a recurrence.
Nutritional Therapy for Hemorrhoids
Nutritional therapy can reduce the pain of hemorrhoids and prevent future ones. One way to prevent the straining that can lead to hemorrhoids is to ensure softer stools. Include unrefined fiber and lots of water and decaffeinated liquids. (Coffee and other drinks with caffeine act as laxatives and can train the colon to be lazy, only producing bowel movements with the help of artificial stimulation.)
Certain nutritional supplements such as vitamin C and the bioflavonoids can strengthen the tone of blood vessel walls and prevent hemorrhoids in other ways. Excess body weight can also make someone susceptible to hemorrhoids, so weight loss is a good idea.
In addition to prevention, nutritional therapy can help ease the pain of hemorrhoids as well. Certain foods, such as coffee, red pepper, mustard, and alcohol, can irritate hemorrhoids as they are passed out of the body. Avoid these.
Consuming sufficient amounts of insoluble and soluble fiber in your daily diet, together with drinking at least eight 8-ounce glasses of water, should eliminate problems with hard stool. Good sources of insoluble fiber include:
- wheat bran
- fruits such as apples and pears
- vegetables such as carrots and spinach
- brown rice
Good sources of soluble fiber include:
- oatmeal or oat bran
- barley
- lentils
- broccoli
Herbal Medicine for Hemorrhoids
Herbs can be used to shrink and strengthen the blood vessels around the anus, providing relief from the pain and bleeding of hemorrhoids. Witch hazel, a native American plant, acts as an astringent when applied to the hemorrhoids. (Be prepared: Witch hazel may sting during the application.) It's often used in distilled or extract form. Another valuable astringent is stone root, often taken in capsule form.
Other herbs commonly used to treat hemorrhoids include:
- bayberry bark
- butcher's broom
- calendula
- ginkgo
- pilewort
- plantain
- horse chestnut
Hydrotherapy for Hemorrhoids
Hydrotherapists use applications of water to ease the pain of hemorrhoids and encourage the circulation of blood in the area around the anus. The types of hydrotherapy commonly used for hemorrhoids are:
- alternating warm and cold sitz baths -- soaking the area
- hot and cold compresses -- alternating applications of comfortably hot and ice-cold washcloths
- cold compresses -- applying ice-cold cloths only
Certain herbs, such as yarrow, can be added to the water in each of these treatments for an astringent effect. Follow these steps for an alternating sitz bath:
- Fill the bathtub with four inches of comfortably warm water.
- Sit in the tub with your knees bent and near your chest.
- Sit for five minutes.
- Refill the tub with cold water.
- Sit in the cold water the same way for one minute.
- Repeat the procedure three times.
Other Hemorrhoid Therapies
- Aromatherapy for Hemorrhoids -- Several essential oils, including cypress, geranium, and myrrh, can be used in sitz baths and as compresses.
- Ayurvedic Medicine for Hemorrhoids -- Treatment can involve dietary changes, stress reduction (including meditation), and herbal therapy (with astringent herbs).
- Detoxification, Fasting, and Colon Therapy for Hemorrhoids -- Fasting can relieve constipation.
- Homeopathy for Hemorrhoids -- Common remedies include nux vomica, belladonna, hamamelis, and collinsonia.
- Yoga for Hemorrhoids -- Yoga offers exercises to relieve constipation and improve circulation.
Piles (Haemorrhoids)
Piles, or haemorrhoids, are areas in the anal canal where the tissue, which contains lots of blood vessels, has become swollen. They can be internal, occurring inside the anus, or external, when they can be seen and felt on the outside of the anus. When visible they look like round pink swellings, the size of a pea or a grape. Piles are common in pregnant women, but are rare in children.
What causes piles?
Straining to empty the bowels when constipated.
Chronic diarrhoea.
Pregnancy – the weight of the fetus on the abdomen and the increased blood flow, as well as the effect of hormones on the blood vessels.
Childbirth – pushing during childbirth increases the pressure in the veins.
Straining to pass urine, especially in men with prostate problems.
Cancer or growths in the pelvis or bowel, which may exert pressure in a similar way to a pregnancy. Family history – piles can run in families and are potentially hereditary, perhaps because of weak veins in the anal area.
Obesity.
Varicose veins – many people with these also develop piles, although piles are not varicose veins.
Different types of piles
Piles are classified according to their position. First-degree piles remain inside the rectum or anal canal. Second-degree piles protrude (or prolapse) from the anus when the bowels are opened, but return of their own accord afterwards. Third-degree piles are similar, but only return inside when pushed back. Fourth-degree piles hang permanently outside the anus.
What are the symptoms?
Most people affected have internal piles and may not have any symptoms at all. The earliest symptom is often bleeding of fresh, red blood from the anal passage when the bowels are opened. There may be itchiness around the anal area. Third and fourth degree piles may be more painful and tend to produce a slimy discharge of mucus that leaks from the exposed lining of the pile.
There are conditions other than piles that can cause bleeding from the anus, so anyone who notices bleeding in their stool should visit a doctor for advice.
Diagnosing piles
The doctor will ask about your health and carry out a physical examination.
If there are external piles, these will be spotted on examination. A rectal examination, where a gloved finger is gently inserted into the anal canal, will be performed. Internal piles cannot normally be felt in this way, but the examination can reveal other problems such as an anal fissure - a painful tear of the lining of the anus. These other conditions need to be excluded before a diagnosis can be made.
Relieving symptoms
Regular warm baths may relieve the irritation; Ice packs may help reduce swelling,
Treatments
Piles can usually be treated at home. The most important element in encouraging existing piles to clear up is to avoid constipation. By having regular bowel movements, and avoiding straining, stools pass easily and do not put pressure on the blood vessels in the anal area.
Eating plenty of fibre-rich foods such as fruit, vegetables and wholegrain cereals (eg brown rice, wholemeal bread), and drinking plenty of fluids, especially water, should keep bowel movements soft.
Avoid rich and spicy food,non-vegtarian food,strict no to pickles
It may help to take a fibre supplement or mild laxatives which soften bowel motions.
Homeopathic treatment for Piles
Homeopathy greatly helps in curing piles specially the 1st 2nd and 3rd degree piles and no surgery should be thought of till homeopathy has been tried. Some of the most commonly used medicines in treating piles are:
Hamamelis –Q –very very useful in controlling bleeding caused due to piles
Aesculus hip-piles with acute pain in the back
Collinsonia..chronic painful bleeding piles with pain as if sticks were placed in the rectum.
Graphitis-for piles and fissures with hard stools
Ratanhia-pain as if splinters of glass were sticking in the rectum
Other commonly used medicines are ..Sulphur,Nux.Vomica,silicea etc.
Subscribe to NewsLetter
Get the latest updates via EmailService provided by FeedBurner